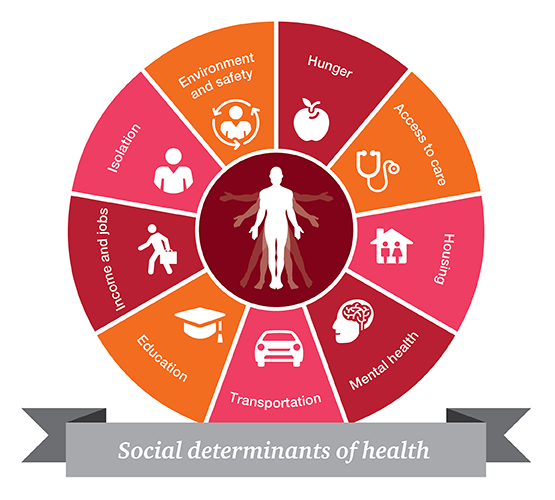
Increasing recognition has been paid to the role that social, economic and environmental factors play in one’s overall health. By addressing issues outside of traditional healthcare, often more cost effectively, overall health outcomes will be improved, cost to the system will be lowered and health disparities reduced. The government and other payers have started to recognize this as a key issue and there will be increasing programs put forth to address this.
Come and learn more about this important topic from a panel of experts: